Carbon County is trying to contact the positive cases of COVID-19 as fast as they come. In an effort to speed up the isolation process, the WDH has created a link for individuals who test positive to use. The positive individual should enter their information into the document and a quarantine letter will be auto generated. They will be able to use this letter for their employers or school. There is also a link for individuals that have been in close contact that need quarantine instructions.
At this time, COVID-19 vaccinations are not being provided at Memorial Hospital of Carbon County or any of our clinic locations. Please contact the Carbon County Public Health at 307-328-2607 for COVID-19 vaccinations.
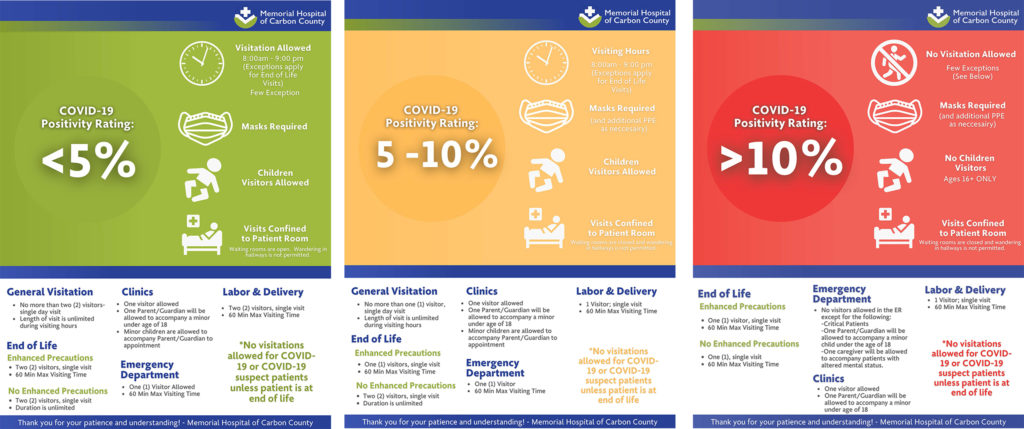
Visitor Guidelines
Visitor restrictions will be based on weekly COVID-19 positivity rates in Carbon County. The following restrictions will be implemented throughout the hospital as well as all MHCC clinic locations.
Hospital Restrictions
As a precautionary measure, Memorial Hospital of Carbon County has put in place the following restrictions:
At each entrance, COVID-19 (Coronavirus) Screening Stations will be in place. ALL employees, visitors, and patients must complete the screening, so that we can best care for you, and protect our patients and staff. Screening stations will be present at each MHCC Clinic as well.
What You Can Expect
- You will be asked a series of questions regarding travel and recent activity.
- MHCC Staff will be performing a temperature check.
- This information will determine the next steps taken.
- Any patient who is checking in should tell staff and ask for a mask if you have a fever, or cold or flu symptoms.
- Visitors with cold or flu symptoms are not allowed to visit any area of MHCC.
Upon completion of the COVID-19 screening, you will be escorted to and from your appointment by a MHCC Staff Member.
We encourage you to get updates at:
Thank you for your cooperation as we work to ensure the safety of all!
Infection Prevention
To prevent the spread of COVID-19, use the same precautions you would for the flu and common cold. MHCC recommends these infection-prevention practices:
- If you’re sick, stay home. Call your provider if you suspect you have the virus.
- Wash your hands often with soap and water for 20 seconds, or use alcohol-based hand sanitizer.
- Cover your mouth and nose with a tissue or your sleeve – not your hands – when coughing or sneezing.
- Clean your home, workspace, shared items, and other frequented locations.
- Avoid unnecessary contact with sick individuals.
- The CDC does not recommend that people who are well wear a face mask to protect themselves from respiratory diseases, including COVID-19.
- Facemasks should be used by people who show symptoms of COVID-19 to help prevent the spread of the disease to others
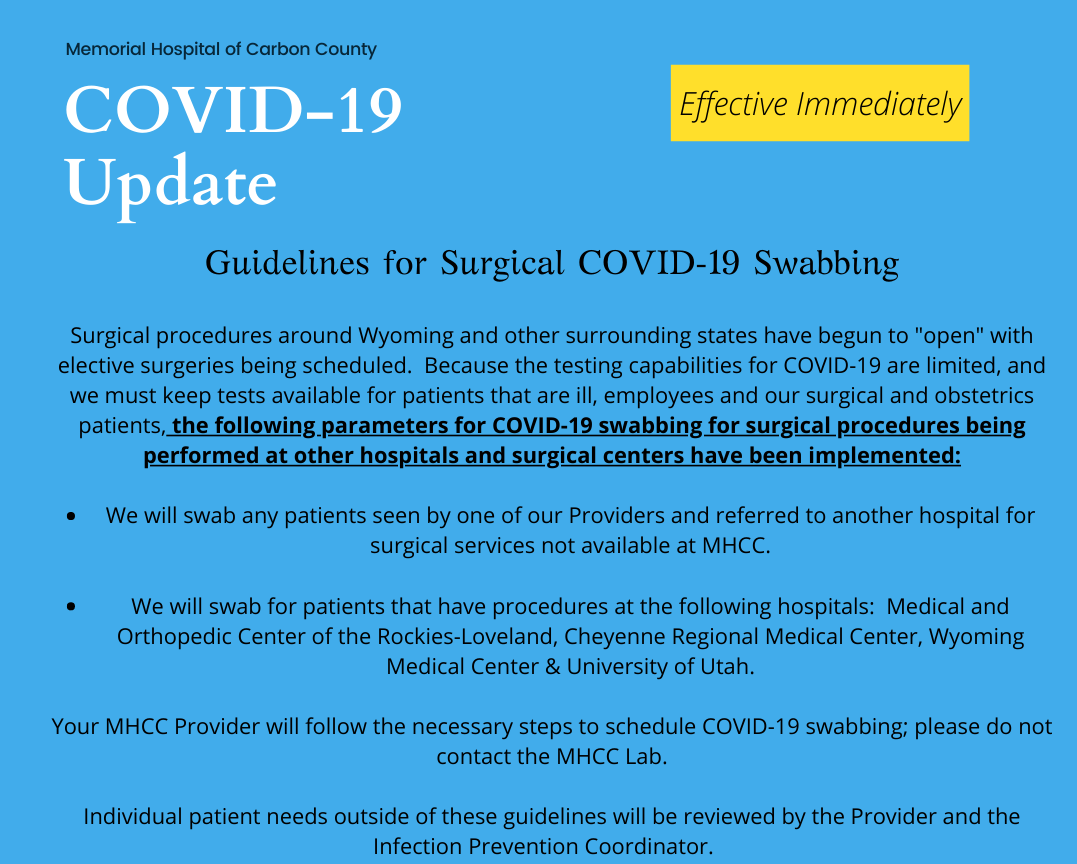
New surgery and procedure policy
Universal Masking
Memorial Hospital of Carbon County requires all employees and patients to wear masks in every patient care environment. Patients are encouraged to arrive for their appointment already wearing a mask. If you do not have a mask, one will be provided for you. Please retain this mask for future visits due to limited supplies.
Well Clinic
Many patients visit Memorial Hospital of Carbon County for regular checkups to ensure continued good health. We have designated a “well clinic” for your convenience. The Visiting Specialists Clinic (formerly known as Wagon Circle,) is seeing patients for routine health appointments with no signs of the virus. Ask your provider or clinic staff.
Virtual Visits
Many primary care and specialty visits can now take place by phone or video chat, so you don’t have to leave home! Call your provider today to learn more!
Appointments Required
To ensure efficiency and safety for our patients and staff, we are requiring appointments for all outpatient services. This includes Lab, Radiology, Physical Therapy, Women’s Clinic, Orthopedic Services and General Surgery. Please call 307-324-2221 to be connected to your outpatient service of choice.
Increased Cleaning of Facilities
A clean facility is always vital, but during the COVID-19 crisis, we are taking even more steps to ensure safe, clean facilities.
Frequently Asked Questions (FAQs)
The following frequently asked questions (FAQs) will be continually updated as we monitor the status of coronavirus (COVID-19) and as we receive questions. In addition, supplemental FAQs and information can be found through the Centers for Disease Control and Prevention and the State of Wyoming Department of Health.
What are coronaviruses?
Coronaviruses are a large family of viruses that are common throughout the world. These viruses, at times, can evolve and infect people, and then spread through human-to-human contact. They are the cause of up to 25 percent of the upper respiratory infections seen each year.
How do you get infected with COVID-19?
Human coronaviruses, including COVID-19, spread just like the flu or a cold — through the air from coughs or sneezes; through close personal contact, like touching or shaking hands; by touching an object or surface with the viruses on it and then touching your face; and occasionally, through fecal contamination.
How do I know if I have COVID-19?
The severity can range from mild to severe illness for confirmed novel coronavirus disease 2019 (COVID-19) cases. It has caused many deaths around the world.
The following symptoms may appear 2 to 14 days after exposure:
- Fever
- Cough
- Shortness of breath
These symptoms alone are not a predictor of COVID-19. Check the Centers for Disease (CDC) guidelines to assess risk.
If you need to visit the emergency department to treat concerning symptoms, call ahead to your local facility and ask for a protective face mask when you arrive.
What can I do to prevent getting sick from COVID-19?
You are at a greater risk of getting seriously ill from the influenza virus than COVID-19. Get a flu shot if you haven’t already.
To prevent the spread of COVID-19, use the same precautions you would for the flu and common cold. MHCC recommends these infection-prevention practices:
- If you’re sick, stay home. Call your provider if you suspect you have the virus and feel you need evaluation for symptoms.
- Wash your hands often with soap and water for 20 seconds or use alcohol-based hand sanitizer.
- Cover your mouth and nose with a tissue or your sleeve – not your hands – when coughing or sneezing.
- Clean your home, workspace, shared items and other frequented locations.
- Avoid unnecessary contact with sick individuals.
- The CDC does not recommend that people who are well wear a face mask to protect themselves from respiratory diseases, including COVID-19.
- Face masks should be used by people who show symptoms of COVID-19 to help prevent the spread of the disease to others and healthcare personnel caring for symptomatic patients.
Do we know how long the virus is living on surfaces?
According to an updated study, this coronavirus (SARS-CoV-2) can remain active and viable for up to 2 to 3 days on inanimate surfaces, including stainless steel, plastics, cardboard (up to 24 hours), glass and copper. Frequent cleaning of high-touch surfaces with most cleaners makes the virus inactivate within one minute.
Should I be wearing a mask?
No. Health officials in the U.S. do not recommend the use of masks among the general public because risk of infection is low and limited to close contacts. It has also not been shown to effectively reduce risk of infection. Face masks should be used by people who show symptoms of COVID-19 to help prevent the spread of disease to others, and by healthcare personnel when evaluating and caring for individuals with symptoms.
Overuse of masks by healthy individuals could reduce the much-needed supply for those who could be contagious. Instead, practice infection-prevention methods and avoid interactions with sick individuals.
Will I have to pay to be tested for coronavirus?
Neither the State nor the CDC are billing for the COVID-19 testing. We anticipate that commercial labs will charge for this test, but do not have information at this time.
Should I go to the Emergency Department?
If you need to call MHCC after hours, contact 307-324-8386.
If you cannot manage your symptoms at home and need to visit the Emergency Department, call ahead to your local facility and ask for a protective face mask when you arrive.
Providers should coordinate with their local Emergency Department or hospital if a patient has severe symptoms.
What should I do if I have recently traveled and am sick?
If you have traveled within the past 14 days and feel sick with fever, cough or are having difficulty breathing, you should call your primary care provider to complete a risk assessment over the phone. They will be able to provide guidance on next steps, if needed. While sick, avoid contact with people, stay home and delay any travel to reduce the possibility of spreading illness to others.
Is there a vaccine for COVID-19?
There is currently no vaccine to protect against COVID-19 and the estimate is that it will be 9-12 months before there might be one. The best way to prevent infection is to avoid being exposed to the virus that causes COVID-19.
Is there a treatment for COVID-19?
There is no specific antiviral treatment for COVID-19. People with COVID-19 can seek medical care to help relieve symptoms. Investigational trials are currently underway, and this could change in the future.
Can people who recover from COVID-19 be infected again?
The immune response to COVID-19 is not yet understood. Patients with COVID-19 are unlikely to be re-infected shortly after they recover, but it is not yet known if patients with COVID-19 become immune once they’ve contracted the virus.
If we have a family member (children, elderly parents) we take care of daily who is showing symptoms should we self-quarantine and work from home for 14 days?
Not unless the family member tests positive for COVID-19. You should monitor yourself for development of any symptoms and if they develop, you should contact your primary care provider to complete a risk assessment screening. At this time, the 14-day isolation is only required after travel to a CDC high-risk area or exposure to a known or suspected COVID-19 patient.
What should we do if we have a family member who is immuno-compromised?
The advice is similar to our general recommendations including the practice of good hand hygiene, frequent cleaning of high-touch items and avoiding close contact with others if they notice symptoms of fever, cough and shortness of breath. Also, consider limiting exposures of yourself and these family members to large gatherings and public events.